All Departments
- Aortic valve stenosis (Aortic stenosis)
- arteriovenous malformations
- Avascular Necrosis
- Best cosmetic dentistry in Iran| Dental Treatment in Iran
- Breast Augmentation in Iran|Breast implant in iran
- Breast Reduction surgery
- Cancer in Iran: oncology in Iran
- Cardiology
- Cataract surgery in Iran
- Cochlear Implant Surgery in Iran
- Cosmetic Laser
- Cosmetic Surgery
- Ear cosmetic surgery
- Eye Care
- Eyelid surgery (Blepharoplasty)
- General Heart Surgery in Iran
- General surgery in Iran
- Glaucoma Treatment In Iran
- Hair Transplant
- Heart valve surgery
- lasik Eye Surgery
- Liposuction
- Non-Surgical Cosmetic procedures in iran
- Organ Transplantation in Iran
- Orthopedic
- Paget disease of bone
- Pediatrics
- Plastic surgery
- Psychiatry
- Radiology
- Rhinoplasty surgery in iran
- Shoulder Replacement Surgery
- SkinCare Treatment
- Spinal cord injury
- urolithiasis procedure in iran
- Urology
- Varicocelectomy
Opening Hours

arteriovenous malformations
What is an arteriovenous malformation (AVM)?
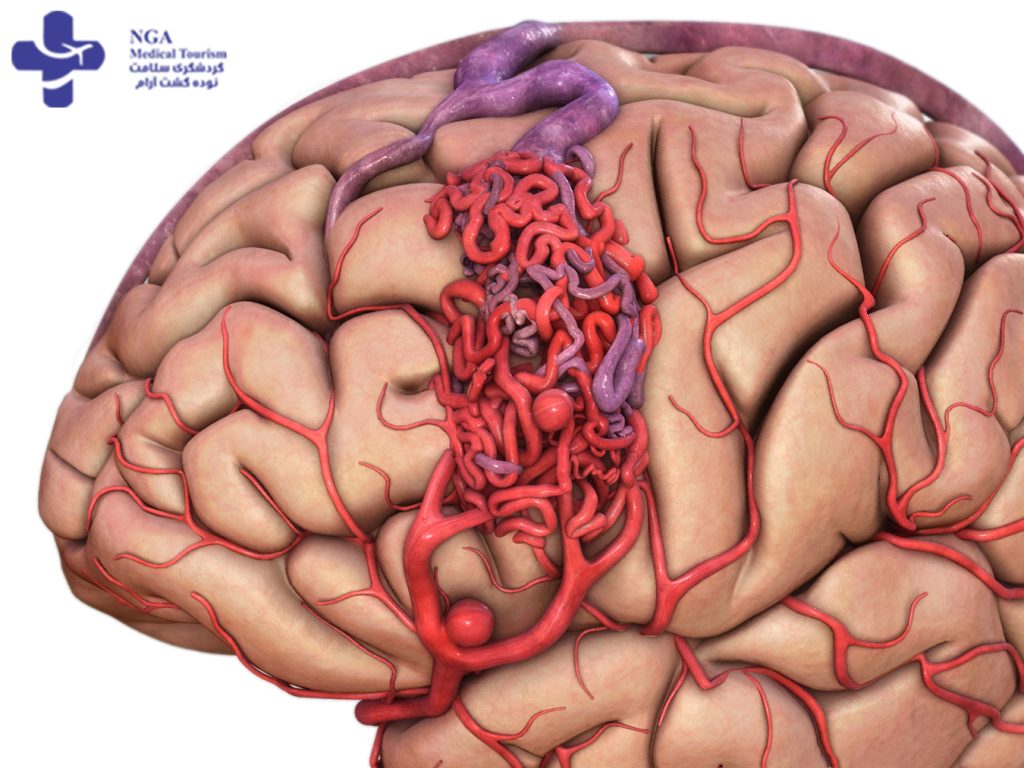
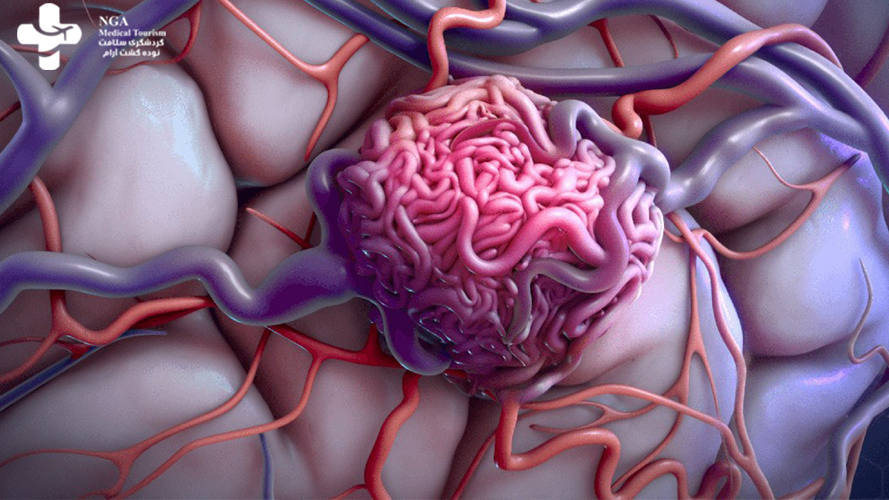
An arteriovenous malformation (AVM) is an abnormal tangle of blood vessels that forms a direct connection between arteries and veins, bypassing the normal capillary network. Normally, oxygenated blood flows from the heart through arteries to capillaries, where it exchanges oxygen and nutrients with the surrounding tissues. The deoxygenated blood then returns to the heart through veins.
In an AVM, the arteries and veins are directly connected without the usual capillary network in between. This can lead to several problems. First, the high-pressure arterial blood flows directly into the low-pressure veins, causing them to enlarge and become weakened. This can result in the formation of dilated, twisted blood vessels called “nidus” within the AVM. Second, the abnormal blood flow can deprive surrounding tissues of oxygen and nutrients, leading to various complications.
arteriovenous malformations treatment
Arteriovenous malformations (AVMs) are abnormal tangles of blood vessels that can occur in various parts of the body, but are most commonly found in the brain and spine. AVMs can cause serious health problems, including neurological symptoms, seizures, and hemorrhages.
The treatment of AVMs depends on several factors, including the size and location of the AVM, the severity of symptoms, and the patient’s overall health. Treatment options include:
1. Observation: Small AVMs that are not causing any symptoms may be observed over time, especially if they are located in a part of the brain that is difficult to access without causing damage.
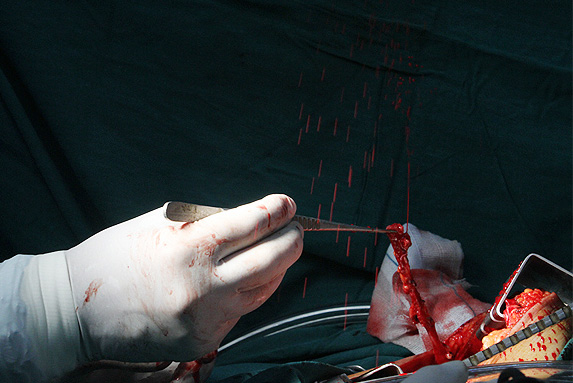
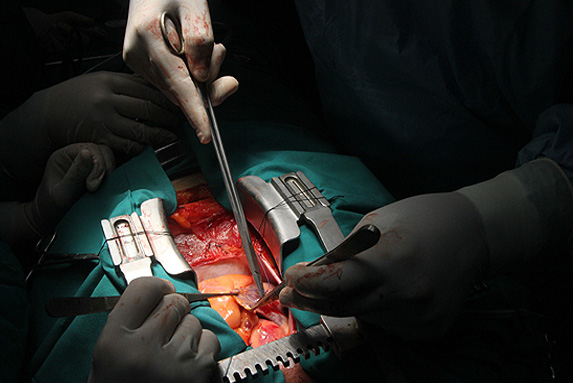
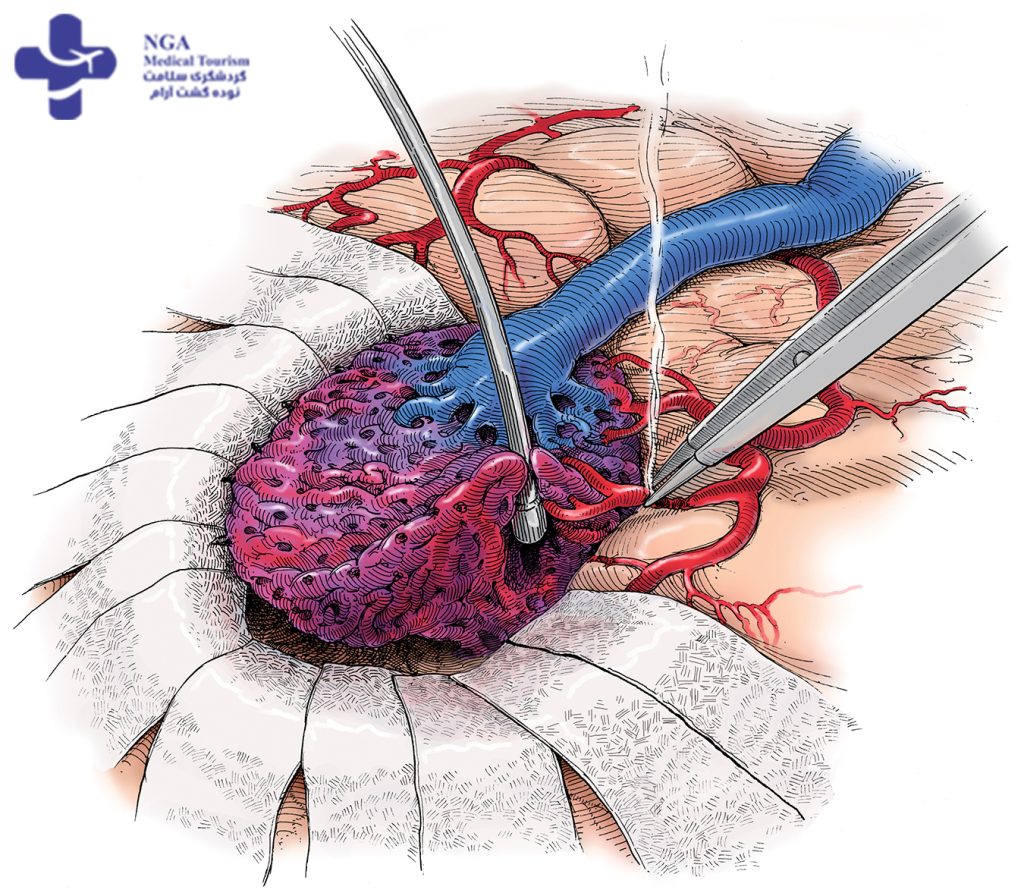
2. Surgery: If the AVM is in a location that can be safely accessed, surgical removal may be an option. The goal of surgery is to remove the AVM completely, which can eliminate the risk of future hemorrhages. However, surgery can be risky and may cause neurological damage.
3. Endovascular embolization: In this procedure, a catheter is inserted into an artery and guided to the AVM. A substance is injected into the catheter that blocks blood flow to the AVM, causing it to shrink over time. This procedure is often used in combination with other treatments.
4. Stereotactic radiosurgery: This is a non-invasive procedure that uses focused radiation to destroy the AVM. The procedure is performed over several sessions and can take several months to be effective.
The choice of treatment depends on many factors, and the decision of which treatment to pursue should be made in consultation with a neurosurgeon or other medical specialist experienced in the treatment of AVMs.
Symptoms of arteriovenous malformations (AVMs) can vary in severity and may include:
Seizures
These can be focal or generalized, involving convulsions, loss of control over movement, or a change in consciousness.
Headache
Headaches associated with AVMs can vary in frequency, duration, and intensity, sometimes resembling migraines.
Pain
Pain can occur on one or both sides of the head. In some cases, the location of the pain may be closely linked to the site of the AVM. Back pain in the lower extremities may also be caused by a spinal AVM.
When AVM ruptures
When an arteriovenous malformation (AVM) ruptures, it means that there is a break or leakage in the abnormal tangle of blood vessels. This rupture can result in bleeding into the surrounding tissues or spaces.
The consequences of an AVM rupture can vary depending on the location, size, and severity of the bleeding. In some cases, the bleeding may be minimal and cause no noticeable symptoms. However, in other instances, it can lead to significant medical emergencies and potentially life-threatening complications.
If an AVM rupture occurs in the brain, it can cause a type of stroke called hemorrhagic stroke. The bleeding puts pressure on the surrounding brain tissue, leading to neurological symptoms such as severe headache, sudden weakness or paralysis, difficulty speaking, vision changes, seizures, loss of consciousness, or even coma.
If the AVM is located in other parts of the body, such as the lungs or liver, rupture can cause internal bleeding, which may result in symptoms like abdominal pain, chest pain, shortness of breath, coughing up blood, or signs of shock.
In the event of an AVM rupture, immediate medical attention is crucial. Emergency medical services should be contacted to ensure rapid evaluation and treatment. Treatment options for AVM rupture may include surgery to stop the bleeding, endovascular techniques to block the bleeding vessels, or supportive care to stabilize the patient while managing the complications.
It is important to note that the information provided here is based on general knowledge and understanding of AVMs and their potential complications. The specific outcome and management of an AVM rupture can vary depending on individual circumstances. Therefore, it is essential to consult with a healthcare professional for accurate diagnosis, evaluation, and appropriate treatment options.

Cerebral arteriovenous malformations (AVMs) are a specific type of AVM that occur in the brain. They are abnormal tangles of blood vessels in the cerebral vasculature, which consists of arteries and veins supplying the brain.
Cerebral AVMs are typically congenital, meaning they are present at birth and develop during fetal development. The exact cause of their formation is not fully understood, but they are thought to result from abnormalities in the development of blood vessels in the brain.
These malformations consist of a complex network of abnormal blood vessels that bypass the normal capillary network. Arteries, which carry oxygenated blood, are directly connected to veins, which carry deoxygenated blood, without the presence of capillaries. This direct connection leads to abnormal blood flow patterns and pressure changes within the AVM.
Symptoms of cerebral AVMs can be diverse and may include:
Headaches: Persistent or severe headaches, often localized to a specific area.
Seizures: AVMs can irritate brain tissue and trigger seizures.
Neurological deficits: Depending on the location of the AVM, neurological symptoms can occur, such as weakness, numbness, difficulty speaking, vision changes, or problems with coordination.
Hemorrhage: The most serious complication is bleeding from the AVM, which can cause a hemorrhagic stroke. Symptoms can include sudden and severe headache, loss of consciousness, vomiting, neurological deficits, or even coma.
Diagnosis of cerebral AVMs involves imaging studies, such as magnetic resonance imaging (MRI), computed tomography (CT) scans, or angiography. These tests help visualize the abnormal blood vessels and determine the size, location, and characteristics of the AVM.

pulmonary arteriovenous malformations
Pulmonary arteriovenous malformations (PAVMs) are abnormal connections between arteries and veins within the lungs. Unlike the normal pulmonary vasculature, which carries deoxygenated blood from the heart to the lungs for oxygenation, PAVMs create direct shunts that allow blood to bypass the capillary network.
PAVMs are typically congenital, meaning they are present at birth, although they may not be diagnosed until later in life. They are associated with certain genetic disorders, such as hereditary hemorrhagic telangiectasia (HHT), also known as Osler-Weber-Rendu syndrome.
The abnormal connections in PAVMs allow deoxygenated blood to bypass the lungs’ oxygenation process and mix with oxygenated blood, reducing the overall oxygen content in the systemic circulation. The severity and consequences of PAVMs can vary depending on their size, number, and location within the lungs.
Symptoms of PAVMs may include:
Dyspnea (shortness of breath): This can occur due to reduced oxygen levels in the blood.
Cyanosis (bluish discoloration of the skin): It can result from decreased oxygen saturation in the systemic circulation.
Fatigue and weakness: Insufficient oxygen delivery to the body’s tissues can cause fatigue and overall weakness.
Recurrent nosebleeds: PAVMs can lead to abnormal blood vessel formations in the nose, resulting in recurrent nosebleeds.
Stroke or brain abscess: In rare cases, PAVMs can allow small blood clots or bacteria to travel from the veins to the arteries, potentially causing stroke or brain abscesses.
Diagnosis of PAVMs involves various imaging studies, such as chest X-rays, computed tomography (CT) scans, or contrast echocardiography. These tests help visualize the abnormal blood vessels and determine the size, number, and location of the PAVMs.
Other vascular lesions that affect the central nervous system
In addition to AVMs, there are three other main types of vascular lesions that can occur in the brain or spinal cord. These lesions differ from AVMs as they involve only one type of blood vessel and do not carry the same high risk of significant hemorrhage. Generally, these low blood flow lesions tend to cause fewer troublesome neurological symptoms and require less aggressive treatment compared to AVMs.
Cavernous malformations
These lesions are formed by clusters of tightly packed, abnormally thin-walled, small blood vessels that displace normal brain or spinal cord tissue. The vessels contain slow-moving or stagnant blood, often clotted or decomposed. Cavernous malformations can vary in size, ranging from fractions of an inch to several inches, depending on the number of blood vessels involved. Some individuals may develop multiple lesions. Due to the fragility of the blood vessel walls, cavernous malformations can occasionally leak blood into surrounding tissues, potentially leading to seizures. After AVMs, cavernous malformations are the most likely type of vascular lesion to require treatment.
Capillary telangiectases
These are clusters of abnormally swollen capillaries that are typically less than an inch in diameter. They are generally benign and rarely cause extensive damage to surrounding brain or spinal cord tissues. Any bleeding that occurs is microscopic in size. However, in certain inherited disorders where individuals develop numerous telangiectases, they can contribute to the development of headaches or seizures.
Venous malformations
These lesions consist of abnormally enlarged veins. They usually do not disrupt blood vessel function and seldom cause hemorrhages. Most venous malformations do not produce noticeable symptoms and often go undetected.
Who is more likely to get arteriovenous malformations?
The exact cause of AVM formation is not fully understood. While most AVMs are present from birth (congenital), they can also develop shortly after birth or later in life. Although there are instances where AVMs are inherited, it is more common for other inherited conditions to increase the risk of developing an AVM. It is estimated that brain AVMs occur in less than one percent of the general population. However, each year, approximately one percent of individuals with AVMs will experience death directly attributed to the AVM.
Causes of vascular lesions
The exact cause of vascular anomalies in the central nervous system is still not well understood. However, scientists believe that these anomalies primarily occur due to developmental errors during embryonic or fetal stages. Genetic mutations are thought to play a role in some cases, suggesting a genetic basis for certain types of vascular malformations. Additionally, there is evidence suggesting that some lesions can be acquired later in life as a result of central nervous system injuries.
During fetal development, the formation and disappearance of blood vessels are continuous processes as the body undergoes changes and growth. These processes are regulated by angiogenic factors, which are chemicals produced by the body to stimulate the formation and growth of new blood vessels. Researchers have identified changes in the chemical structures of angiogenic factors in individuals with AVMs or other vascular abnormalities in the central nervous system. However, it is not yet fully understood how these chemical changes lead to alterations in blood vessel structure.
Through the study of familial patterns, researchers have identified a genetic mutation on chromosome 7 that causes a specific type of cavernous malformation characterized by the formation of multiple lesions. This mutation is found in various ethnic groups but is particularly prevalent among Hispanic Americans in the Southwest region, who share a common ancestor in whom the genetic change originated. Other types of vascular defects in the central nervous system are associated with larger hereditary medical syndromes, such as hereditary hemorrhagic telangiectasia, Sturge-Weber syndrome, and Klippel-Trenaunay syndrome.
arteriovenous malformations treatment
Diagnosing AVMs
Clinicians often use a distinctive auditory sign called a bruit to aid in the diagnosis of an AVM. A bruit is a rhythmic, whooshing sound caused by the abnormally fast blood flow through the arteries and veins of the AVM. It is similar to the sound of water rushing through a narrow pipe. When the bruit is particularly severe and audible to the individual, it can cause hearing impairment, sleep disturbances, or significant psychological distress.
Various imaging technologies are available to detect the presence of AVMs:
- Cerebral angiography (cerebral arteriography) provides the most accurate visualization of the blood vessel structure in brain AVMs. A contrast agent, a special water-soluble dye, is injected into an artery to highlight the blood vessels, which can then be observed on X-rays.
- CT scans (computed axial tomography) use X-rays to create detailed images of the head, brain, or spinal cord. They are particularly useful in identifying hemorrhage.
- MRI (magnetic resonance imaging) uses magnetic fields and radio waves to produce high-resolution images that can reveal subtle changes in neurological tissues.
- Magnetic resonance angiography (MRA) captures the flow pattern and velocity of blood within vascular lesions, as well as the circulation of cerebrospinal fluid in the brain and spinal cord.
- Transcranial Doppler ultrasound is capable of diagnosing medium to large-sized AVMs and determining the presence and extent of hemorrhage. It assesses blood flow in the brain by emitting high-frequency sound waves through the skull toward specific arteries. The resulting sound wave signals, which bounce back from blood cells, are interpreted by a computer to create an image depicting the velocity of blood flow.
These imaging techniques play a crucial role in the diagnosis and evaluation of AVMs, enabling clinicians to assess the size, location, and characteristics of the vascular anomaly.
Treating AVMs
AVM Treatment Options:
AVMs require careful monitoring for signs of instability that may indicate an increased risk of hemorrhage.
Treatment options include medication for symptom management, surgery, or focused radiation therapy.
Venous malformations and capillary telangiectases rarely require surgery. Cavernous malformations can be surgically removed but have a lower risk of hemorrhage.
Treatment decisions are made on a case-by-case basis, considering the risk of hemorrhage and potential complications of surgery.
An AVM grading system helps estimate surgical risk based on AVM size, location, and involvement.
Three surgical options are available: conventional surgery, endovascular embolization, and radiosurgery.
Conventional surgery removes the central portion of the AVM through open surgery, suitable for superficial AVMs.
Endovascular embolization involves injecting substances to create an artificial blood clot within the AVM, used in conjunction with surgery or radiosurgery.
Radiosurgery uses focused radiation to damage and close the blood vessels of small AVMs.
Embolization and radiosurgery may have incomplete results and potential risks, but they provide treatment options for deeply situated AVMs.
Combining staged embolization, surgery, and radiosurgery can further reduce complications and improve outcomes.
What are the latest updates on arteriovenous malformations?
In collaboration with Columbia University’s medical school, NINDS has established a long-term study group to understand the natural progression of AVMs and enhance surgical treatments. The ARUBA study demonstrated that medical management alone is superior to combined medical management and interventional therapies for unruptured brain AVMs. Ongoing research aims to study risk factors for bleeding in individuals with hereditary hemorrhagic telangiectasias (HHT) and explore anti-angiogenic therapy using drugs like Apo-Timop. Non-human models are being used to investigate gene-related mechanisms of AVM formation. Biomarkers for AVM risk assessment and molecular pathways involved in AVM development are also under investigation. Excessive expression of vascular endothelial growth factor (VEGF) may contribute to brain AVMs, and researchers are studying the use of adeno-associated virus to prevent abnormal blood vessel formation. Studies on cerebral cavernous malformations (CCMs) have identified potential therapeutic targets related to structural proteins and the Rhoa/ROCK protein signaling pathway.
FAQ about Arteriovenous Malformation (AVM)
Arteriovenous malformations (AVMs) are abnormal tangles of blood vessels that connect arteries and veins. They can occur in the brain, spinal cord, or other parts of the body.
Arteriovenous malformations (AVMs) are relatively rare. It is estimated that AVMs occur in less than 1% of the general population.
It is difficult to provide an exact number of people who have arteriovenous malformations (AVMs) worldwide due to variations in prevalence and underdiagnosis. However, based on estimates, it is believed that AVMs occur in less than 1% of the general population. Considering the global population of over 7.9 billion people, the number of individuals with AVMs would be in the millions. It’s important to note that these numbers are estimates and may vary.
AVMs can be cured through surgery, radiation therapy, or embolization. Surgery involves removing the AVM, redirecting blood flow. Radiosurgery uses focused radiation to close off the blood vessels over time. Embolization blocks blood flow with materials inserted into the AVM. Success depends on AVM characteristics and individual response. Combining treatments may be necessary. Consultation with a knowledgeable medical professional is crucial for determining the best approach.
Liver transplant
A liver transplant is a surgery that removes a liver that no longer functions properly (liver failure) and replaces it...
Kidney transplant
A kidney transplant is a surgery to place a healthy kidney from a living or deceased donor into a person whose kidneys...
Ischemic Heart Disease
Ischemic means that an organ (e.g., the heart) is not getting enough blood and oxygen. Ischemic heart disease, also...
Heart Bypass Surgery
Heart bypass surgery has been a life-saving treatment for more than 60 years.It is the most frequently performed openheart..
Heart Transplant
In heart transplant surgery, the patient’s heart is replaced by a natural heart from a donor who
Open Heart Surgery
Open (traditional) heart surgery is when the chest is cut open and surgery is performed on the...
Angioplasty
Coronary angioplasty is a treatment intended to fix narrowed or clogged arteries with the aim of enhancing blood ...