Thyroidectomy Surgery in Iran
Best Hospital
We Introduce Best Hospital for Thyroidectomy Surgery
Best Doctors
We Introduce Best Doctors for Thyroidectomy Surgery
Best Price
We Try to introduce best Services with Regular Price
Why choose Iran for treatment and medical procedures?
• Low costs
• Board licensed surgeons
• Quality health care
• Less waiting time
• Accredited hospital
• Personal service
• Language capability
• Ease of medical visa
• Treatment with advanced technology
• Strong presence in advanced healthcare e.g. Transplantation - high success rate in the operation.
Active clinics for international patients:
Shahid Dastani Clinic, Hematology, Oncology and Stem Cell Transplant Clinic, Nuclear Medicine Clinic and Special Clinic.
Clinics: urology, nephrology, lung, general surgery, endocrinology, gastroenterology, gynecology, midwifery, perinatal, infertility, maxillofacial surgery, genetics, dermatology, orthopedics, neurosurgery, heart, heart surgery, vascular surgery, neurology, rheumatology, ear and Otorhinolaryngology, dentistry, infectious, speech therapy, pain, nutrition and diet therapy, anesthesia, celiac disease, liver cirrhosis, Behcet, eye, psychiatry, men’s health
Paraclinical departments: clinical laboratory, pathology, imaging and pharmacy
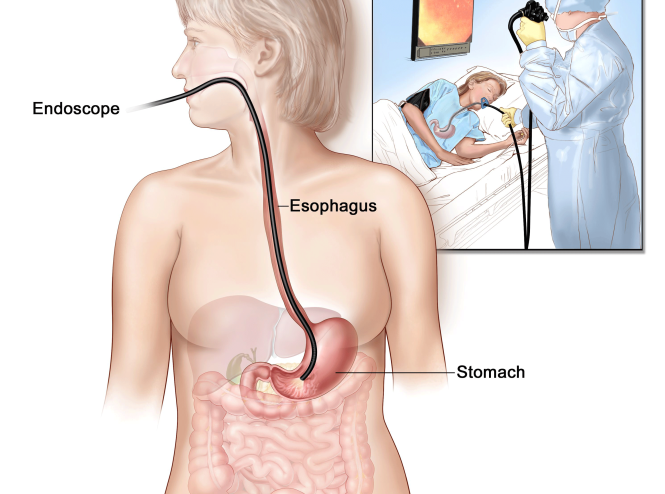
Clinics: EMG-EEG, bronchoscopy, spirometry, bone densitometry, nuclear medicine, dialysis, physiotherapy, endoscopy, echocardiography, exercise test, pain control, rehabilitation and sports medicine.
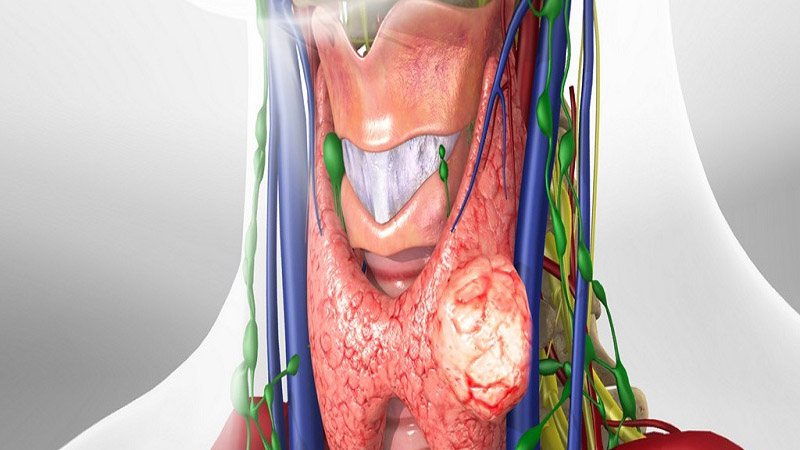
Thyroidectomy is surgery to remove all or part of the thyroid gland. It is indicated in various thyroid pathologies: thyroid cancer, cancerous or large volume nodule, compressive goiter, etc.
Thyroidectomy cost | thyroid surgery cost
Thyroidectomy is surgery to remove all or part of the thyroid gland. It is indicated in various thyroid pathologies: thyroid cancer, cancerous or large volume nodule, compressive goiter, etc.
What is thyroidectomy?
Thyroidectomy involves the partial or total removal of the thyroid.
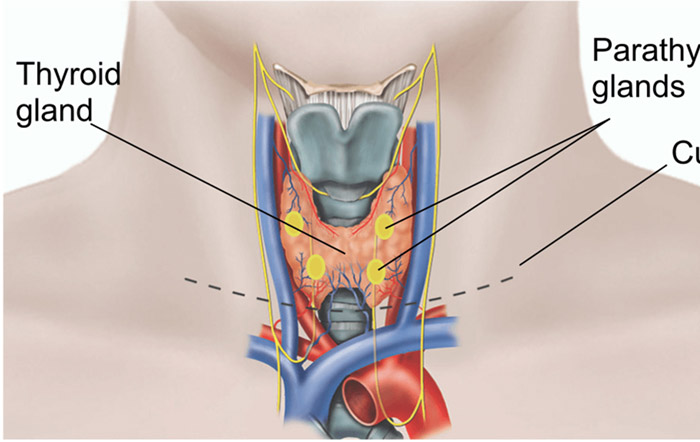
Gland made up of two globes (hence its butterfly shape) located at the base of the neck, under Adam’s apple, the thyroid regulates the rate of metabolism of many organs, via the T3 and T4 hormones that she secretes. It therefore plays a very important role in our body.
How is the thyroidectomy performed?
The operation takes place under general anesthesia. It lasts from 40 minutes to 1h30. The patient is placed on the back, the head slightly extended.
The surgeon makes a horizontal incision of a few centimeters at the base of the neck. He then proceeds to the resection of the thyroid, partial or total depending on the indication of the intervention.
In the event of simple nodule resection, a microscopic examination called “extemporaneous examination” is carried out during the intervention in order to verify the exact nature of the nodule removed. Depending on the result, the surgeon may be required to perform a more extensive ablation than that initially planned.
At the end of the procedure, a small drain is left in place, then the incision is usually closed using staples, which give the best aesthetic results.
When to perform a thyroidectomy?
Thyroidectomy is indicated in various pathologies of the thyroid:
in the event of a doubtful or cancerous thyroid nodule: the thyroid nodule is a swelling that develops in the thyroid tissue. Frequent, particularly in women over 50, it is most often benign. In 5% of cases however, it is cancerous. On certain warning signs (risk factors, size and ultrasound characteristics of the nodule, TSH level), a cytopuncture will be performed to verify the nature of the nodule. If the result is reassuring, simple monitoring of the nodule by ultrasound is sufficient. If the results show a doubtful character, an ablation of the thyroid lobe is indicated;
in the presence of a benign nodule whose large volume (more than 25 mm in diameter) causes difficulty in swallowing, breathing and/or speaking;
Thyroidectomy Surgery in Iran
in the event of compressive goiter (increase in the volume of the thyroid) causing difficulty in swallowing and breathing;
in case of thyroid cancer;
in case of multinodular goiter: multiple nodules develop in the two thyroid lobes, within a thyroid itself increased in volume (goiter). A thyroidectomy may be necessary if the nodules are large, if they present a suspicious character to the cytopuncture or if the goiter causes compression;
in certain cases of so-called “hot” or “toxic” thyroid nodules, i.e. secreting a large quantity of thyroid hormones and therefore causing hyperthyroidism;
in case of Graves’ disease, autoimmune disease causing hyperthyroidism. In case of relapse after a first drug treatment, surgery is sometimes proposed.
Depending on the indication, the resection will be more or less extensive. We thus distinguish:
simple resection of the nodule: only the nodule is removed, the rest of the thyroid is preserved;
a lobectomy or lobo-isthmectomy: only one lobe of the thyroid is removed. It’s the most frequent case ;
a “sub-total” thyroidectomy: only a fragment of the thyroid gland is left in place on each side;
a total thyroidectomy: the thyroid is completely removed;
total thyroidectomy with lymph node dissection, more rare, for certain thyroid cancers.
Today, medical teams have the most conservative attitude possible.
After thyroidectomy
The postoperative course
The postoperative course is not very painful and easily relieved by analgesic treatment if necessary. Food can be resumed the day after the operation. The first half of the staples are removed the day after the operation, the other half before discharge. The scar is left in the open air, without a dressing, and it is not recommended to wet it for ten days.
ospitalization lasts 2 to 3 days
In the event of total thyroidectomy, daily replacement therapy with thyroid hormones is necessary for life. It is started during hospitalization and subsequently balanced by the attending physician or endocrinologist. This replacement therapy may also be necessary after partial removal if the secretion of thyroid hormones is insufficient.
Depending on the extent of the thyroid removal, the possible replacement therapy and the nature of the professional activity, the work stoppage can last up to 3 weeks.
The scar is located in the natural folds of the neck, so it is usually not very visible. But it all depends on the quality of the healing, which varies from person to person.
The risks and complications
Thyroidectomy is a simple procedure with very rare complications: hematoma, hemorrhage, respiratory discomfort, infection.
Different disorders can appear, most often transiently:
difficulty swallowing;
dysphonia (change in the pathway) due to recurrent nerve damage during the procedure and which may require, in some cases, speech therapy;
swelling in the operated area;
a disruption of calcium regulation that can cause tingling and cramps, due to damage to one or more parathyroid glands (glands involved in calcium regulation) during the procedure. Calcium and vitamin D supplementation (necessary to fix calcium) is sometimes necessary.
Thyroidectomy is a type of surgical intervention on the thyroid gland, which implies its complete removal with the development of persistent postoperative hypothyroidism.
The thyroid gland is distinguished by a wide variety of pathogenetically different diseases, such as colloid, proliferating goiter to varying degrees, adenomas, chronic autoimmune thyroiditis, Graves’ disease (diffuse toxic goiter), malignant tumors of the thyroid gland, requiring various therapeutic approaches, in some cases, a decision on surgical treatment.
The history of the development of modern thyroid surgery is no more than 130-140 years. The danger and complexity of performing thyroid surgery has been discussed by surgeons of all generations. As early as 1928, the surgeon De Quervain wrote “… whoever, not having a good surgical background, succumbs to the temptation to operate on some kind of” light “goiter, should not forget about cases that, in inexperienced hands, ended in death from blood loss on the operating table.”
Surgical treatment of thyroid diseases developed rapidly in the second half of the 19th century due to the introduction of general anesthesia methods. The founders of thyroid surgery were the Austrian surgeon Albert Theodor Billroth and the Swiss surgeon Emil Theodor Kocher.
Theodor Kocher was an active supporter of total thyroidectomy in patients with goiter. Kocher’s skill made it possible at that time to reduce mortality in such operations from 38% to 0.3%. After performing the first operation in 1874, his clinic until 1882 was the main medical center in Europe for surgical interventions on the thyroid gland. It was Theodor Kocher who in 1883 described the condition of myxedema that develops after the removal of the thyroid gland, which he called “Cachexia thyreopriva”. In 1909, Kocher received the Nobel Prize in Physiology or Medicine in recognition of his significant contributions to the pathophysiology and surgery of the thyroid gland.
At the same time, in 1883, the surgeon and naturalist from Geneva, Jacques Louis Reverdin, published an article on the development of myxedema after total thyroidectomy – “Mixoedeme postoperatoire”. Until that moment, the relationship between myxedema and the consequences of thyroidectomy had not been established. It is Reverdin who was the first to discover and substantiate this fact, therefore both Kocher and Reverdin are considered the discoverers of postoperative hypothyroidism.
Cancer Treatment in Iran
The most common cancer treatment in Iran is chemotherapy, but ...
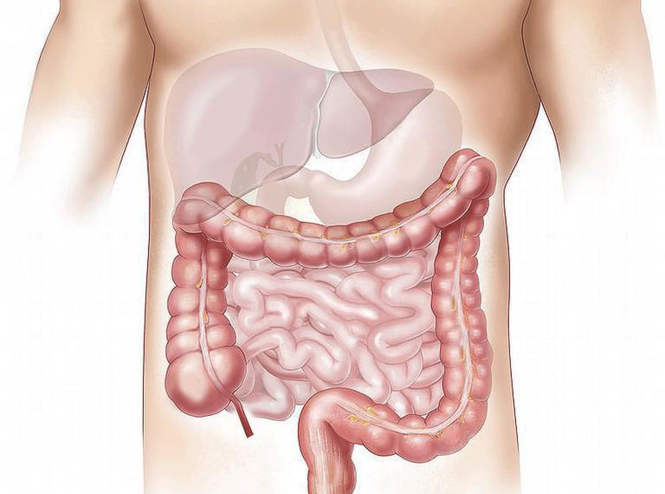
Colon Cancer Treatment in Iran
The treatments for colorectal cancer usually involve surgery to remove the cancerous tumor
Stomach Cancer Treatment in Iran
The most common types of stomach cancer treatment are surgery ,chemotherapy...
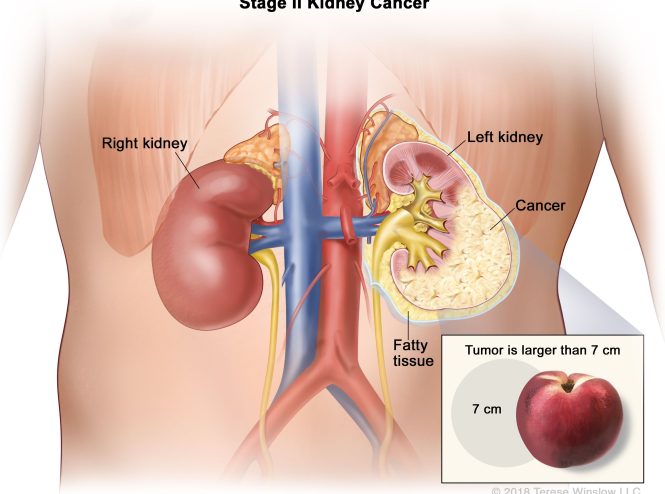
Kidney Cancer Treatment in Iran
Kidney cancer is usually treated with surgery, targeted therapy, immunotherapy ...
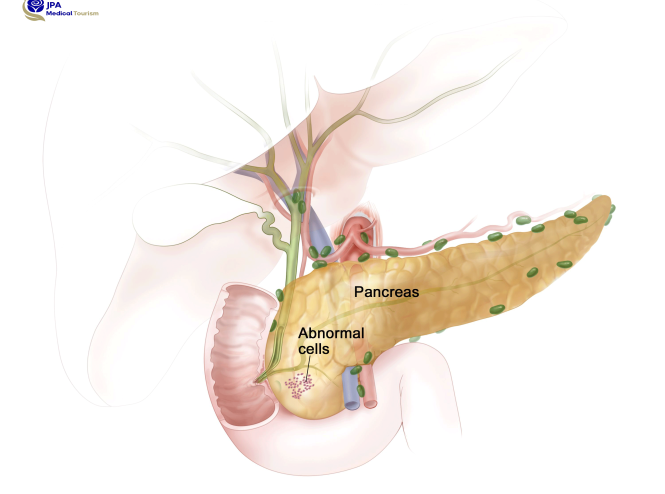
Pancreatic Cancer Treatment in Iran
Pancreatic cancer treatments are surgery, chemotherapy, or a combination of them
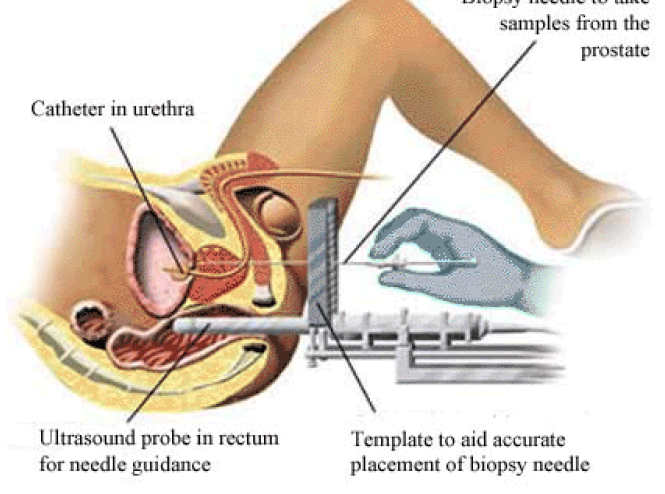
prostate surgery in Iran
The most effective cancer treatments are surgery and localized treatments
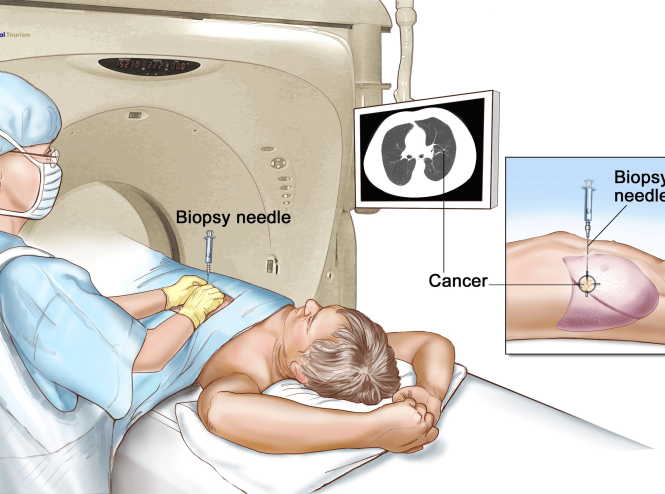
Lung Cancer Treatment in Iran
Lung cancer can be treated with surgery, chemotherapy, radiation therapy, targeted therapy ...
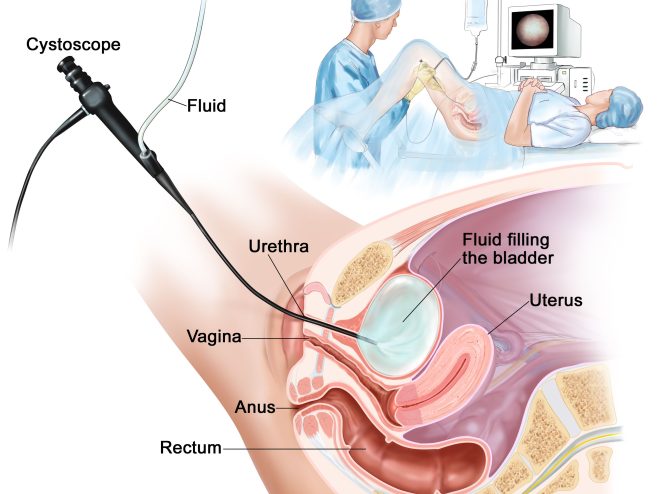
Bladder Cancer Treatment in Iran
Bladder cancer is usually treated using surgery, Chemotherapy, radiation, or immunotherapy.
Contract party with child-friendly medical centers
- The first successful heart transplant center in Iran
- The first bone marrow transplant center in Iran
- The first kidney transplant center in Tehran
- The first center to perform CT Scan in Iran
- The first center for video capsule endoscopy in Iran
- Referral center for the treatment of blood and oncology diseases and the treatment of blood cancers with bone marrow transplantation
- A reputable center for fellowship training in bone marrow transplantation, hematology and oncology in the country
- Establishing non-relative stem cell bank (connected to world stem cell bank)
- Scientific pole of nuclear medicine of the country
- Cancer treatment referral center with radiopharmaceuticals
- The only training center approved by the International Atomic Energy Agency
- Iran nuclear medicine association center
- Center equipped to treat digestive and liver diseases
- The only center performing the POEM technique in the treatment of gastrointestinal diseases in the country
- Superspecialized center for the treatment of gastrointestinal problems, including advanced diagnostic and therapeutic ERCP, with the technique of combining two technical methods, “endoscopy” and “fluoroscopy”.
- One of the world’s most prestigious centers in the field of maxillofacial surgery and the use of 3D printers
- The only fetal laser surgery treatment center in the Middle East
- A reputable center in the treatment of female infertility and IVF in the country
- The scientific hub of rheumatology treatment in the country
- Specialized vascular angiography services in the treatment of diabetic foot
- Orthopedic subspecialty services (knee joint replacement, spinal correction surgeries for children in the country)
Considering that the patient should be examined first and the necessary tests should be done to determine the grading and staging of his disease, and based on that, it is decided what measures should be taken for treatment and surgery.
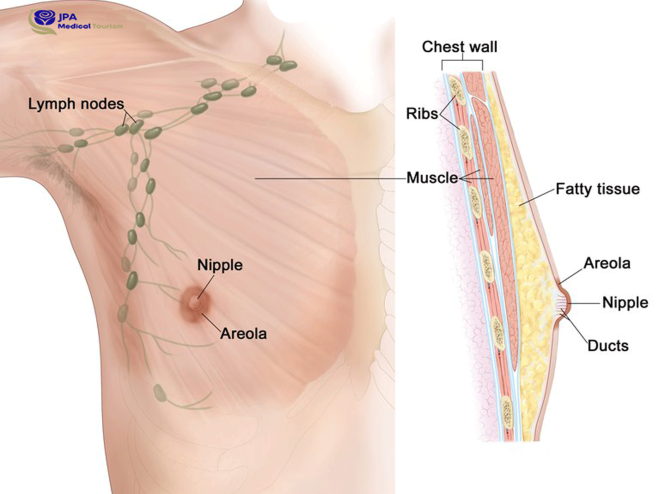
Call for more information on prices for breast surgery
If the patient is in a high grade of the disease, or has metastasized and involved other organs of the body, or if there is an infected person in the close people and relatives of the patient, it means that the patient has a genetic and family tendency to advance and relapse. In this case, two breasts are often operated.
For many years, one of the main unresolved issues of thyroid surgery has been the choice of the extent of surgical intervention on the thyroid gland. At the same time, the complexity of compensation that occurs after surgery for hypothyroidism was the main obstacle to complete removal of the thyroid gland. For a long time, the lack of drugs, the impossibility of dosing accuracy in replacement therapy led to the difficult achievement of stable euthyroidism after surgery. This was the impetus for the choice of organ-preserving surgical tactics when performing operations on the thyroid gland.
Until the middle of the 20th century, the treatment of hypothyroidism involved the administration of animal thyroid extracts to patients. These preparations, in which it was practically impossible to accurately dose the content of thyroid hormones, could not sufficiently provide stable euthyroidism, and their administration itself was accompanied by significant difficulties. In 1913, Nobel Prize-winning American biochemist Edward Kelvin Kendall isolated, purified crystallized thyroxine and achieved a 100-fold increase in the concentration of hormones in thyroid extracts, which served as a turning point in the creation of modern thyroxin preparations. The creation of precisely dosed synthetic preparations of thyroid hormones radically changed the idea of the treatment of thyroid diseases and led to a revolution in thyroidology, expanding the possibilities of thyroid surgery.
In our region, until 1995, to compensate for postoperative hypothyroidism, an extract of the dried thyroid gland, thyroidin, was used, which was titrated only by the total iodine content, and most of the clinical presentations were formed in a period when there were no modern preparations of levothyroxine (L-T4). In this regard, in relation to any disease of the thyroid gland, there was a postulate that hypothyroidism is a severe complication of these diseases. The expansion of the possibility of performing operations on the thyroid gland obliged endocrinologists to develop strict indications for surgical methods for the treatment of thyroid diseases, in order to avoid excessive operational activity.
Why jahan pakhsh aram in iran?
- Low cost
- Board Certified Surgeons
- Quality Health Care
- Less Waiting Time
- Accredited Hospital
- Personalized Services
- Language Capability
- Ease of Medical Visa Facilitation
- Advance Technology Treatment
- Strong presence in advanced healthcare e.g. Organ Transplant – High success rate in operations.
Absolute indications for thyroidectomy are all forms of malignant tumors of the thyroid gland. Considering the situation of the post-Chernobyl period and the post-accident consequences, total thyroidectomy is recognized as the method of choice even for minimally invasive, highly differentiated thyroid carcinomas. Mandatory preoperative cytological verification of the diagnosis makes it possible to determine the scope of the planned surgical intervention. Performing a total thyroidectomy for highly differentiated thyroid carcinomas opened up opportunities for effective treatment of metastases with 131I isotopes and made it possible to achieve favorable treatment results.
Most often, surgical interventions on the thyroid gland are performed for nodular goiter. It should be noted that modern thyroidology has a wide range of diagnostic methods (ultrasound, cytological, hormonal, radiological) that make it possible to determine the pathogenetic and morphological basis of the disease before treatment and, in most cases, avoid surgical intervention, recognizing the minimum oncological risk of detected focal changes in the thyroid gland. In most cases, nodular goiter is represented by colloidal, to varying degrees, proliferating goiter (up to 90%), which is subject to observation and conservative treatment. Operative interventions of an organ-preserving nature in multinodular colloid proliferating goiter usually lead to a relapse of the disease, and there must be good objective reasons for thyroidectomy.
Indications for surgical treatment in patients with nodular goiter are:
cytologically confirmed carcinomas;
neoplasms suspicious of a malignant nature;
cases of complex cytomorphological diagnosis (follicular and B-cell tumors – the frequency of malignancy in this group reaches 30%);
local compression syndrome of the neck organs with large benign neoplasms;
thyrotoxicosis with nodular and multinodular goiter of large size.
The most debatable issue is the choice of the volume of surgical intervention in Graves’ disease (diffuse toxic goiter). Before the pathogenesis of Graves’ disease was elucidated, the ideology of surgical treatment of this disease was as follows: in a patient with thyrotoxicosis, an increase in the size of the thyroid gland was most often detected, and in order to normalize the level of thyroid hormones, part of the organ must be removed. The most common operation was and still is – subtotal resection of the thyroid gland according to O.V. Nikolaev. Later it became obvious that Graves’ disease is a systemic autoimmune disease that develops as a result of the production of antibodies to the thyroid-stimulating hormone receptor (AT-rTSH), and leaving a part of the thyroid gland during subtotal resection is leaving a target for stimulating antibodies in the body, which leads to relapse. thyrotoxicosis. Therefore, the only predictable outcome and goal of surgical treatment for Graves’ disease is the removal of the entire thyroid gland. In this regard, according to modern concepts of recent times, hypothyroidism has ceased to be considered as a complication of surgical intervention in Graves’ disease and has actually become the goal of treatment.
According to the literature of recent years, subtotal resections of the thyroid gland for Graves’ disease are logically (based on the pathogenesis of the disease) and practically unjustified. In most foreign clinics, the operation of choice for Graves’ disease, the “gold standard”, has become thyroidectomy.
In the last decade, a large number of works devoted to the problem of hypothyroidism have appeared, which have transformed our views on thyroid diseases. First of all, this is due to the introduction of modern thyroid hormone preparations into clinical practice. Against the background of taking these drugs, hypothyroidism becomes for the patient not a disease, but a way of life that practically does not imply any special restrictions. Modern precisely dosed synthetic preparations of levothyroxine (L-T4) do not differ in structure from human thyroxine (T4) and make it possible to easily and effectively maintain stable euthyroidism against the background of their administration only once a day.
The prerequisites for this are factors such as:
The only vital function of the thyroid gland is the production of thyroid hormones;
The daily rhythm of secretion of thyroid hormones is practically absent (the variation from day to day is less than 15%), and therefore, the daily intake of levothyroxine (L-T4) in the same dose easily models their endogenous production;
The stability of the body’s need for thyroid hormones (rare situations in which a change in the selected dose of L-T4 is required are pronounced changes in body weight, pregnancy and the parallel administration of certain drugs);
High bioavailability of L-T4 when taken orally;
Long plasma half-life of L-T4 (about 7 days);
The presence of an exact criterion (TSH level), which fully reflects the quality of hypothyroidism compensation for a long period (about 2-3 months);
Relative cheapness of L-T4 preparations;
The quality of life of patients with hypothyroidism who constantly receive L-T4 replacement therapy practically does not differ significantly from that of those without hypothyroidism.
The goal of substitution therapy for hypothyroidism is to maintain a stable level of thyroid hormones in the body that meets physiological needs. The main indicator to assess the adequacy of replacement therapy for hypothyroidism is the level of TSH, determined by methods with high functional sensitivity.
The principles of replacement therapy for hypothyroidism are well known. The international guidelines for the laboratory diagnosis of thyroid diseases summarize them quite succinctly:
Levothyroxine (L-T4) preparations are preferred for hypothyroidism replacement therapy.
Euthyroidism in adults is usually achieved by administration of L-T4 at a dose of 1.6 mcg/kg body weight per day. The need for L-T4 in children is much higher and can reach 4 mcg/kg per day. The initial dose of the drug and the time to reach the full replacement dose is determined individually, depending on age, body weight and the presence of concomitant heart disease.
The need for L-T4 decreases with age. Some older people may receive less than 1 mcg/kg L-T4 per day.
The need for L-T4 increases during pregnancy. Evaluation of thyroid function in pregnant women, which involves the study of the level of TSH and free T4, is advisable in each trimester of pregnancy. The dose of L-T4 should be sufficient to maintain normal TSH and free T4 levels.
In postmenopausal hypothyroid women on estrogen replacement therapy, an increase in L-T4 dose may be necessary to maintain normal TSH levels.
The goal of replacement therapy for primary hypothyroidism is to maintain the TSH level within 0.5 – 1.5 mU / l.
TSH levels slowly change after changing the dose of L-T4 or prescribing a different drug; it is examined no earlier than 6-8 weeks after the appointment of a full replacement dose.
To assess the adequacy of the dose of L-T4, 2-3 months after the appointment of a full replacement dose, it is necessary to determine the level of TSH. If the TSH level remains elevated, the L-T4 dose should be increased by 25 mcg, followed by TSH control after 6-8 weeks.
Patients receiving a titrated dose of L-T4 are advised to have their TSH levels checked annually. The level of TSH is not affected by the time of blood sampling and the interval after taking L-T4. If, in addition to this, the determination of the level of free T4 is used to assess the adequacy of therapy, the drug should not be taken in the morning before blood sampling, since for about 9 hours after taking L-T4, the level of T4 in the blood is significantly increased (by 15 – 20%).
Ideally, L-T4 should be taken on an empty stomach 30 to 40 minutes before meals, at the same time of day, and at least 4 hours apart before or after other medications or vitamins.
Taking drugs and compounds such as cholesterol, ferrous sulfate, soy proteins, sucralfate, and antacids containing aluminum hydroxide, which reduce the absorption of L-T4, may require an increase in its dose.
Today, the most widespread synthetic preparations of levothyroxine – “Eutiroks” company Nycomed. The drug has proven itself in practical use, is easily dosed, and with the right dosage does not cause side effects.
After radical treatment of highly differentiated thyroid carcinomas, patients should undergo suppressive therapy with thyroid hormone preparations aimed at correcting postoperative hypothyroidism and suppressing TSH-dependent growth of residual tumor cells. The drug of choice is levothyroxine (L-T4); the use of triiodothyronine (liothyronine L-T3) is unacceptable for long-term treatment and is limited to short courses of preparing a patient for scintigraphy with 131I. For most patients, the achievement of suppression of the TSH level to the minimum detectable numbers in the range of 0 – 0.05 mU / l is shown. TSH levels are controlled at least 3 months after initial treatment. The dose of L-T4 is further adjusted by decreasing or increasing it by 25 mcg / day with repeated monitoring of serum TSH after 3 months. When the optimal dosage of L-T4 is reached, there is no need to control the level of free T4 and free T3 in the blood serum, and the level of TSH is monitored every 6-12 months. In patients with an undoubted remission of the disease during treatment, suppressive therapy is recommended for 3–5 years.
Side effects in the form of subclinical thyrotoxicosis are most often manifested by cardiac symptoms and osteopenia. Retrospective studies have shown that these effects are minimal when an appropriate dose of L-T4 is selected and carefully monitored to avoid excess blood levels of free T4 and free T3. However, in elderly patients or in patients with cardiac pathology that aggravates the patient’s condition, it is possible to refrain from conducting suppressive therapy. It should be borne in mind that during subclinical thyrotoxicosis, the prothrombin profile is disturbed in most patients.
It is also important to control calcium metabolism in patients who have undergone thyroidectomy. In some cases, transient parathyroid insufficiency that occurs in the first 6-12 months after surgery should be compensated by taking calcium supplements (Calcium D3 Nycomed) in combination with the active form of vitamin D (Tahistine, α – D 3) in individually selected doses.