All Departments
- Aortic valve stenosis (Aortic stenosis)
- arteriovenous malformations
- Avascular Necrosis
- Best cosmetic dentistry in Iran| Dental Treatment in Iran
- Breast Augmentation in Iran|Breast implant in iran
- Breast Reduction surgery
- Cancer in Iran: oncology in Iran
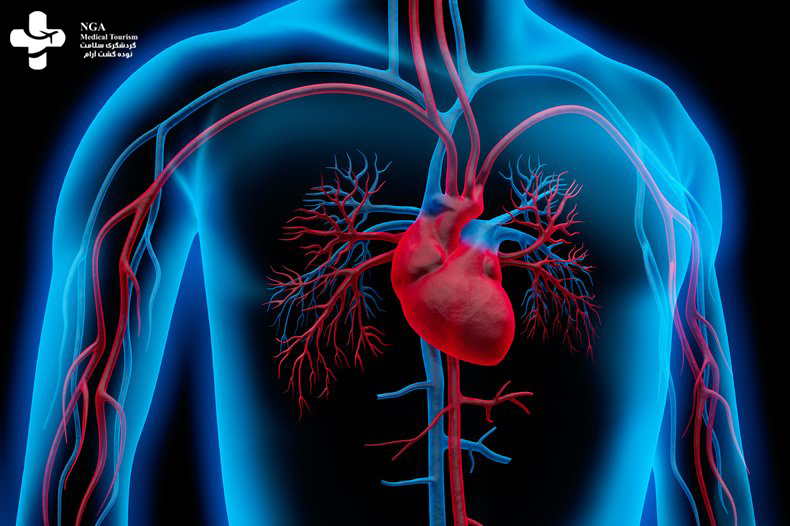
- Cardiology
- Cataract surgery in Iran
- Cochlear Implant Surgery in Iran
- Cosmetic Laser
- Cosmetic Surgery
- Ear cosmetic surgery
- Eye Care
- Eyelid surgery (Blepharoplasty)
- General Heart Surgery in Iran
- General surgery in Iran
- Glaucoma Treatment In Iran
- Hair Transplant
- Heart valve surgery
- lasik Eye Surgery
- Liposuction
- Non-Surgical Cosmetic procedures in iran
- Organ Transplantation in Iran
- Orthopedic
- Paget disease of bone
- Pediatrics
- Plastic surgery
- Psychiatry
- Radiology
- Rhinoplasty surgery in iran
- Shoulder Replacement Surgery
- SkinCare Treatment
- Spinal cord injury
- urolithiasis procedure in iran
- Urology
- Varicocelectomy
Opening Hours

Aortic valve stenosis (Aortic stenosis)
Angiography is a medical imaging technique used to visualize the blood vessels in the body, particularly the arteries and veins.Angiography is a medical imaging technique used to visualize the blood vessels in the body, particularly …
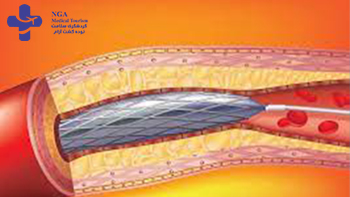
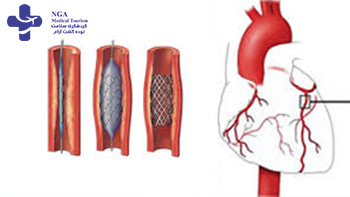
Angioplasty is a medical procedure used to treat narrowed or blocked blood vessels, typically arteries, and restore blood flow to the affected area. It is often performed as a follow-up to an angiography procedure when a blockage or narrowing is detected.

Heart bypass surgery, also known as coronary artery bypass graft (CABG) surgery, is a surgical procedure performed to improve blood flow to the heart muscle when the coronary arteries are severely blocked or narrowed. It is typically …

Open heart surgery, also known as cardiac surgery, is a surgical procedure performed on the heart with the chest cavity opened. It involves accessing the heart directly to treat various conditions or perform corrective procedures.

Heart transplant surgery, also known as cardiac transplantation, is a surgical procedure in which a diseased or failing heart is replaced with a healthy heart from a deceased donor. It is typically performed on patients …
Aortic aneurysm surgery is a procedure performed to repair or treat an aortic aneurysm, which is an abnormal bulging or dilation of the aorta, the largest artery in the body. Aortic aneurysms can occur in different sections…
Heart pacemaker surgery, also known as pacemaker implantation, is a procedure performed to treat abnormal heart rhythms or electrical conduction disorders. A pacemaker is a small electronic device that helps regulate the…
Aortic Valve Stenosis
Aortic valve stenosis, also known as aortic stenosis, is a medical condition characterized by the narrowing of the aortic valve in the heart. The aortic valve controls the flow of blood from the heart’s left ventricle to the aorta, which is the main artery that carries oxygenated blood to the body. In aortic stenosis, the narrowing of the valve restricts the blood flow, causing the heart to work harder to pump blood. This condition can lead to symptoms such as chest pain, shortness of breath, fatigue, and fainting. Aortic valve stenosis can be caused by age-related degeneration, congenital heart defects, or certain medical conditions. Treatment options may include medication, valve repair, or valve replacement surgery, depending on the severity of the condition. Early diagnosis and management of aortic stenosis are crucial to prevent complications and improve the patient’s quality of life.
What is aortic valve stenosis?
Aortic valve stenosis, or aortic stenosis, refers to the narrowing or blockage of the aortic valve in the heart, disrupting the normal blood flow and potentially leading to serious health complications, including heart damage and even death. This condition restricts the amount of oxygen that your body receives due to impaired blood flow. As a result, individuals with aortic stenosis may experience symptoms such as chest pain, shortness of breath, and fainting. Early detection and appropriate management are vital in order to prevent further complications and improve overall well-being.
Who does aortic valve stenosis affect?
Aortic stenosis is primarily observed in the elderly population and its prevalence increases significantly after the age of 65. However, certain diseases can lead to the development of aortic stenosis in middle-aged individuals as well. In rare cases, infants can be born with a congenital defect in the aortic valve, resulting in stenosis. It is important to consider age and underlying conditions when diagnosing and managing aortic stenosis, as appropriate treatment plans can vary based on individual circumstances. Regular medical check-ups and screenings are crucial in detecting and addressing this condition in a timely manner.
How common is aortic valve stenosis?
Approximately 2% of individuals over the age of 65 in the United States are affected by aortic stenosis to varying degrees. Unfortunately, a significant number of people are unaware of their condition until symptoms manifest or it is incidentally detected through screenings or diagnostic tests. This highlights the importance of regular medical evaluations, particularly for older individuals, to promptly identify and manage aortic stenosis to improve outcomes and prevent complications. Early detection and intervention play a critical role in ensuring appropriate medical care for individuals with this condition.
What causes aortic stenosis?
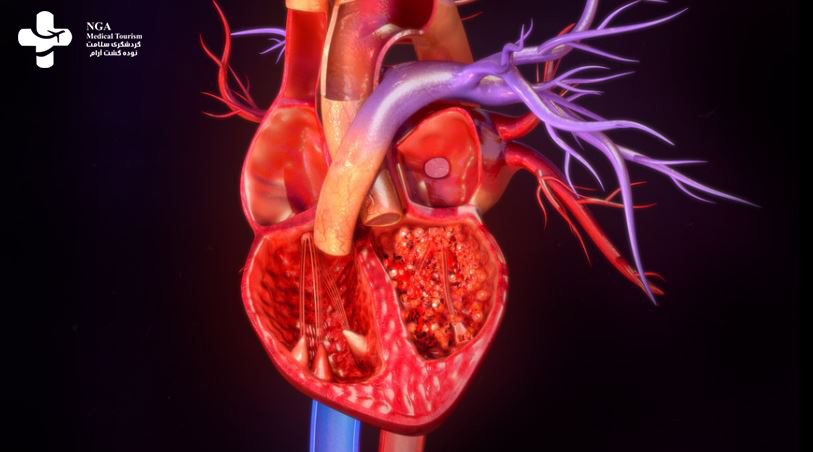
The aortic valve is one of the four valves present in the heart. Positioned as the final gateway for blood before it is pumped out to the body, this valve normally consists of three leaflets that open to allow blood to pass through and close tightly to prevent any backward flow into the previous chamber.
Insufficiency occurs when the aortic valve fails to allow an adequate amount of blood to flow through. In some cases, the valve is unable to seal tightly, resulting in regurgitation, where blood flows in the wrong direction. Both conditions lead to an accumulation of excess blood in the final heart chamber, causing increased pressure and placing additional strain on the heart. This can potentially lead to heart damage and necessitate increased effort by the heart to function properly.
Aortic stenosis in adults has three main causes:
Aortic valve stenosis can be caused by various factors, including:
- Wear and tear due to age: With time, calcium deposits can accumulate on the valve, similar to the process of atherosclerosis in blood vessels. This buildup restricts blood flow through the valve, leading to stenosis. Age-related aortic stenosis is more common in individuals over the age of 65.
- Damage from infections: Untreated infections, particularly strep throat or scarlet fever, can introduce bacteria into the bloodstream. These bacteria may then settle on the heart valves, triggering an immune response that damages the valve. This can result in aortic stenosis, with the development of such conditions typically associated with rheumatic fever. The effects of this damage may take years or even decades to become evident.
- Caused by other inherited or chronic conditions: Certain rare conditions, such as Paget’s disease of the bone, kidney failure, and familial hypercholesterolemia, have been linked to the development of aortic valve stenosis. Additionally, autoimmune or inflammatory diseases like lupus and rheumatoid arthritis have been associated with an increased risk of aortic stenosis.
These factors contribute to the progression of aortic valve stenosis by impairing the normal function and structure of the valve, leading to narrowing and reduced blood flow through the aortic valve.
What are the symptoms of aortic stenosis?
The symptoms of aortic stenosis can vary in severity and may include:
- Fatigue: Feeling tired, especially when it interferes with your regular activities or occurs during activities that previously did not exhaust you.
- Heart palpitations: Sensation of being aware of your own heartbeat, which can be unpleasant.
- Swelling in the feet, ankles, or lower legs: Accumulation of fluid in the lower extremities.
- Chest pain (angina): Discomfort in the chest, which can feel like squeezing, pressure, or discomfort. The pain may radiate to the neck, jaw, arm, or abdomen.
- Shortness of breath: Difficulty breathing or feeling breathless, particularly during physical exertion or when lying flat.
- Dizziness, lightheadedness, or fainting: Feeling dizzy or lightheaded, and in some cases, experiencing fainting episodes.
How fast does the condition progress?
Aortic stenosis can progress at different rates, with some individuals experiencing a gradual onset over several years, while others may experience a more rapid progression. It is important not to delay treatment as waiting too long can lead to irreversible damage to the heart and an increased risk of sudden death in cases of severe aortic stenosis.
Due to the potential risks associated with untreated or advanced aortic stenosis, healthcare providers may strongly advise against delaying treatment. Seeking timely medical intervention and following the recommended treatment plan can help manage the condition effectively and reduce the risk of complications.
How is aortic stenosis diagnosed?
If your primary care provider suspects that you have aortic stenosis, they may refer you to a cardiologist for further evaluation. The cardiologist will employ various diagnostic tests to confirm the diagnosis and assess the severity of the condition. These tests may include:
- Physical exam: The doctor will examine you for signs of swelling in the lower legs and ankles, and listen to your heart sounds using a stethoscope. The presence of a heart murmur is often indicative of aortic stenosis.
- Electrocardiogram (ECG or EKG): This test measures the electrical activity of your heart through sensors attached to your chest. It can provide valuable information about the functioning of your heart.
- Imaging tests:
- Chest X-ray, angiography, or cardiac CT scan: These methods use X-rays to visualize the structures inside your body. Contrast dye may be used to enhance the images, enabling a better view of the heart and blood vessels.
- Echocardiogram: This non-invasive test uses ultrasound waves to create images of your heart. It provides detailed information about the structure and function of the heart, including the aortic valve.
- Transesophageal echocardiogram (TEE): This specialized type of echocardiogram involves inserting a device into your mouth and down your esophagus to obtain clearer images of the heart and surrounding blood vessels.
- Heart MRI: This imaging technique uses a powerful magnetic field to generate detailed scans of the heart, providing comprehensive information about its structure.
- Exercise stress testing: This test measures your heart’s function while you are physically active, helping determine the presence and severity of aortic valve stenosis.
- Cardiac catheterization: In this procedure, a thin tube is inserted into an artery, typically in the groin, and guided to the heart. It allows for direct visualization of the heart and assessment of aortic stenosis. Additionally, it provides information about the heart’s overall function.
These diagnostic tests assist the cardiologist in confirming the diagnosis of aortic stenosis, evaluating its severity, and planning an appropriate treatment strategy.
Can aortic stenosis be cured?
The treatment options for aortic stenosis depend on the severity of the condition and the presence of symptoms. Your healthcare provider will recommend an appropriate treatment approach, which may include:
- Medication: For milder cases of aortic valve stenosis without symptoms, medications such as blood thinners or drugs to treat heart rhythm disorders may be prescribed to manage the condition.
- Valve repair: In cases where the damage is limited and regurgitation is minimal, valve repair procedures can be considered. There are two main options:
- Aortic valve surgery: This surgical procedure involves making an incision in the chest to directly access and repair the valve. It can be performed using traditional or minimally invasive techniques.
- Balloon valvuloplasty: In this procedure, a catheter with a balloon at the tip is inserted into an artery and guided to the heart. The balloon is then inflated to widen the narrowed aortic valve. Balloon valvuloplasty is typically used in select cases to alleviate symptoms temporarily until valve replacement is feasible.
- Valve replacement: When valve repair is not feasible or appropriate, valve replacement is considered. There are several methods available:
- Aortic valve surgery: Similar to valve repair, this procedure involves replacing the damaged valve with a new one. The replacement valve can be a donor valve (typically from an animal source), a mechanical valve, or a bioprosthetic valve.
- Ross procedure: In this procedure, your own pulmonary valve is used to replace the damaged aortic valve. A donor valve is then used to replace the pulmonary valve.
- Transcatheter aortic valve replacement (TAVR): This minimally invasive procedure allows for valve replacement without open-heart surgery. A catheter-based device is inserted into an artery and guided to the heart to replace the aortic valve. In some cases, a “valve-in-valve” approach is used to place the new valve directly over the existing one.
What types of replacement valves are there, and why choose one over the others?
Human donor valve: These valves are obtained from organ and tissue donors. They are frozen and stored until needed. Human donor valves are a suitable option for individuals who cannot or prefer not to take blood-thinning medications for an extended period. However, these valves have a lifespan of around 15 to 20 years and may require replacement in the future.
Animal valve: Valves made from animal tissue, usually sourced from pigs or cows, are another option. Like human donor valves, they do not require long-term blood-thinning medications. Animal valves also have a lifespan of approximately 15 to 20 years before they may need to be replaced.
Mechanical valve: Mechanical valves are made from durable materials such as pyrolytic carbon, with some models featuring polyester knit fabric around the edges. These valves are long-lasting and well-tolerated by the body. However, if you receive a mechanical valve, you will need to take blood thinners for the remainder of your life to prevent complications like stroke. Mechanical valves are designed to last a lifetime.
Bioprosthetic valve: Bioprosthetic valves combine animal tissue with artificial components. The animal tissue is typically attached to a metal frame to ensure proper placement. These valves have a lifespan similar to human and animal valves, lasting around 15 to 20 years.
What else can I do to manage aortic stenosis?
For individuals with no symptoms or mild aortic stenosis, regular monitoring and follow-up appointments are typically sufficient. Those with moderate stenosis may need to limit physical activity and take medications. Severe aortic stenosis warrants evaluation for aortic valve replacement or repair. Medication may be required temporarily or permanently, and your healthcare provider will provide specific instructions. Regular communication with your healthcare provider is essential for proper management.
aortic valve stenosis icd 10
The ICD-10 code for aortic valve stenosis is I35.0. This code falls under the category of “Nonrheumatic aortic valve disorders” and is used to indicate a diagnosis of aortic valve stenosis, which is a narrowing of the aortic valve in the heart. The ICD-10 code is used by healthcare providers and insurance companies to help with billing and reimbursement for medical services related to the treatment of aortic valve stenosis.
6 months after aortic valve replacement
Six months after aortic valve replacement surgery, most patients are well on their way to recovery and are able to resume many of their normal activities. However, the recovery process can vary depending on the individual and the type of surgery performed.
During the first few weeks after surgery, patients typically need to take it easy and avoid strenuous activities. They may also need to attend follow-up appointments with their healthcare provider to monitor their progress and ensure that the new valve is functioning properly.
As the weeks and months progress, patients may gradually increase their activity level and return to normal daily activities. However, it is important to avoid heavy lifting, contact sports, and other activities that could put stress on the new valve.
Patients may also need to make some lifestyle changes to protect their new valve and reduce their risk of further heart problems. This may include adopting a heart-healthy diet, quitting smoking, and engaging in regular exercise.
Overall, six months after aortic valve replacement surgery, most patients are able to resume many of their normal activities and enjoy a good quality of life. However, ongoing care and monitoring by a healthcare provider are important to ensure the continued health and function of the new valve.
nonrheumatic aortic valve stenosis
Nonrheumatic aortic valve stenosis refers to a narrowing of the aortic valve that is not caused by rheumatic fever, a condition that can cause damage to the heart valves. Instead, nonrheumatic aortic valve stenosis can be caused by a variety of factors, including congenital heart defects, age-related changes to the heart valve, and other medical conditions such as high blood pressure, high cholesterol, or diabetes.
Symptoms of nonrheumatic aortic valve stenosis may include chest pain, shortness of breath, fatigue, and lightheadedness. In severe cases, it can lead to heart failure and sudden cardiac death.
Treatment for nonrheumatic aortic valve stenosis may involve medication to manage symptoms, but in severe cases, surgical intervention may be necessary. This can include aortic valve replacement surgery, which involves removing the damaged valve and replacing it with an artificial valve.
Prevention of nonrheumatic aortic valve stenosis can include adopting a heart-healthy lifestyle, including regular exercise, a heart-healthy diet, and avoiding smoking and excessive alcohol consumption. It is also important to manage other medical conditions that can contribute to the development of aortic valve stenosis, such as high blood pressure, high cholesterol, and diabetes.
Overall, early detection and appropriate treatment are key to managing nonrheumatic aortic valve stenosis and preventing complications.
How long does it take to recover from this treatment?
The recovery period for aortic valve stenosis repair or replacement varies depending on the specific method employed. Surgical procedures generally have longer recovery times, with patients spending several days in the hospital and requiring several weeks for full recovery.
On the other hand, transcatheter methods such as balloon valvuloplasty and TAVR have shorter recovery periods. In some cases, individuals undergoing these procedures can be discharged on the same day or the following day and resume their normal activities shortly thereafter.
Can aortic stenosis be prevented?
Aging-related aortic stenosis is typically unavoidable, but maintaining a healthy lifestyle, including a balanced diet, maintaining a healthy weight, and regular exercise, can help prevent other cardiovascular diseases.
Preventing aortic stenosis caused by bacterial infections primarily involves prompt treatment of these infections, including following prescribed antibiotics and medications until fully recovered.
Inherited or chronic condition-related aortic stenosis is generally not preventable. Congenital aortic valve stenosis, which occurs from birth, cannot be prevented.
What is the outlook for aortic stenosis?
Untreated aortic stenosis can have significant negative impacts on one’s life, particularly when it reaches a severe or critical stage. Without treatment, most individuals do not survive beyond a few years.
Delayed treatment of aortic stenosis can yield mixed outcomes, depending on the extent of permanent heart damage. The prognosis worsens as the damage increases. While partial recovery may be possible, full recovery is unlikely.
Timely or early treatment of aortic stenosis leads to a positive or excellent prognosis. Lifelong follow-up care is necessary, but individuals can generally resume their normal activities.
When should I call my healthcare provider after I go home?
If you decide not to pursue treatment for aortic stenosis or if you have not received treatment yet, it is important to contact your healthcare provider if any of the following situations occur:
- Development of a new symptom related to aortic stenosis or a sudden worsening of existing symptoms.
- Symptoms begin to significantly disrupt your daily life and activities.
When should I go to the ER?
If you have recently started a new medication, it is important to seek emergency medical attention by going to the emergency room if any of the following occur:
- Experience an unexpected or severe side effect from the medication. Your healthcare provider can inform you about which side effects require immediate medical attention.
- Faint or lose consciousness for any reason.
- If you are taking blood thinners and experience a fall. Blood thinners significantly increase the risk of internal bleeding, particularly after a fall or other injury, which can be life-threatening.
After undergoing surgery or a catheter procedure, it is advisable to go to the emergency room if any of the following circumstances arise:
- The surgical incision site becomes red, swollen, or hot to the touch, indicating a possible infection that requires prompt treatment.
- Experience any severe symptoms associated with aortic stenosis, such as shortness of breath, chest pain, heart palpitations, or loss of consciousness.
- If you are taking blood thinners and experience a fall, for the same reasons mentioned above related to the increased risk of bleeding.
Overview
Aortic valve stenosis is a serious medical condition that occurs when the aortic valve in the heart becomes narrowed, resulting in restricted blood flow from the heart to the rest of the body. This can lead to a range of symptoms, including chest pain, shortness of breath, fatigue, and lightheadedness.
Treatment for aortic valve stenosis may involve medication to help manage symptoms, but in severe cases, surgical intervention may be necessary. This can include aortic valve replacement surgery, which involves removing the damaged valve and replacing it with an artificial valve.
With appropriate treatment, many people with aortic valve stenosis are able to manage their symptoms and maintain a good quality of life. However, if left untreated, aortic valve stenosis can lead to serious complications, including heart failure and sudden cardiac death.
FAQ about Aortic valve stenosis
Chest pain: A sensation of tightness in the chest and lungs, particularly during physical exertion.
Fatigue: Overwhelming tiredness experienced during periods of increased activity.
Shortness of breath: Difficulty breathing deeply, especially following physical exertion.
Mild: Minimal narrowing of the aortic valve, usually asymptomatic.
Moderate: Increasing narrowing of the valve, mild symptoms during physical activity.
Severe: Significant valve narrowing, pronounced symptoms even with minimal exertion.
Critical: Severe valve narrowing, severe symptoms at rest, requiring immediate treatment.
Call your doctor about new or worsening symptoms, including:
- Chest pain or tightness.
- Rapid fluttering heartbeat.
- Shortness of breath.
- Dizziness or faintness.
- Increased exhaustion after activity.
- Swollen ankles and feet.
- Difficulty sleeping.
Aortic stenosis is a critical and potentially life-threatening condition characterized by the abnormal narrowing, thickening, and stiffening of the aortic valve. This results in restricted blood flow from the ventricle to the aorta.
An echocardiogram is a diagnostic test that utilizes sound waves to generate images of the heart’s movement. It provides valuable information about blood flow through the heart and its valves. This test can detect a weakened heart muscle and assess the extent of aortic valve stenosis.
Classic symptoms of aortic stenosis include dyspnea (shortness of breath), symptoms of heart failure, angina (chest pain), and syncope (fainting). The appearance of these symptoms indicates the presence of hemodynamically significant aortic stenosis and is a crucial factor in determining appropriate management strategies.
In cases of symptomatic severe aortic stenosis (SAS), the preferred treatment is surgical aortic valve replacement (SAVR). However, in elderly patients, the risk associated with surgery can sometimes outweigh the potential benefits.
Acquired aortic stenosis refers to the condition that develops after birth. It is the more common type of aortic stenosis and can be caused by degenerative changes or complications of rheumatic fever.