Liver transplant in Iran: Procedures and Costs
Iran has become a leading hub for liver transplants, with cutting-edge medical facilities and a stellar reputation for transplantation excellence. The healthcare system has made remarkable progress, emphasizing organ transplant procedures. A key contributor to Iran’s liver transplant success is its robust infrastructure and a network of well-established transplant centers.
Iranian medical professionals pioneer innovative transplant techniques, ensuring top-tier care for liver transplant recipients. The expertise of Iranian surgeons, coupled with advanced medical technology, has significantly improved success rates. Global patients view Iran as a viable option for liver transplants due to affordable and accessible medical services.
The Iranian government’s dedication to promoting organ donation has alleviated the organ shortage. Initiatives to raise awareness and streamline transplantation processes have positively impacted organ availability. Iran stands as a beacon of hope for those in need of life-saving liver transplants, showcasing the nation’s commitment to advancing global healthcare.
How expensive is a liver transplant? How much does a liver transplant cost in Iran? Which country does the most liver transplants? Which city in Iran is liver transplant center? What is the success rate of liver transplantation? What characteristics should a liver transplant donor have? How is the liver transplant performed? What are the criteria for a liver transplant? What is the survival rate of liver transplantation based on age? Stay with us to answer these questions and more.
What is a liver transplant?
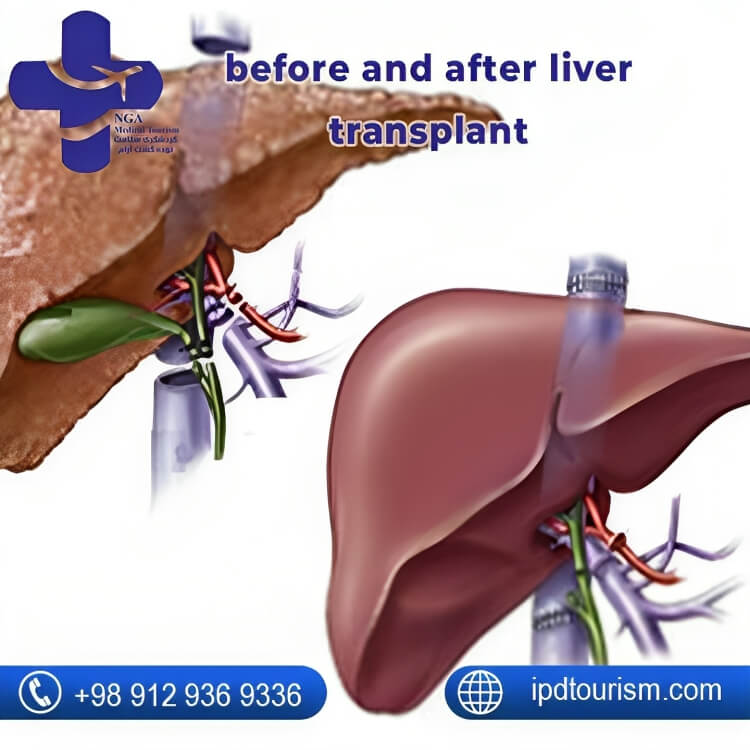
Liver transplantation is a surgical procedure that entails replacing a diseased or damaged liver with a healthy liver from a donor. This intricate medical intervention is typically recommended for individuals confronting end-stage liver diseases, such as cirrhosis, liver failure, or specific liver cancers. The transplantation process involves meticulously matching a suitable donor liver, whether from a deceased or a living donor, to the recipient. During surgery, the medical team removes the damaged liver and implants the healthy donor liver, establishing connections to blood vessels and bile ducts. Post-transplant, healthcare professionals closely monitor patients to manage potential complications and ensure the body accepts the new organ.
What does living donor liver transplant mean?
A living donor liver transplant is a medical procedure in which a portion of a healthy person’s liver is surgically removed and transplanted into a person whose liver is not functioning properly. The donor and the recipient are usually relatives or individuals with a close relationship.
The liver has the remarkable ability to regenerate, so both the donated portion and the remaining portion in the donor’s body can grow back to near-normal size and function. This procedure is often done when a recipient is in need of a liver transplant, and there is a willing and compatible living donor available.
It’s a complex and intricate medical process, but the idea is to provide a new, functional liver to someone in need without relying on organs from deceased donors. This can increase the chances of a successful transplant and reduce the time a recipient has to wait for a suitable organ.
Liver transplant success rate
The success rate of liver transplantation depends on several factors, including the patient’s overall health, age, and the underlying cause of liver failure. Advances in surgical techniques and medical care have significantly improved outcomes in recent years. Careful post-surgery management and strict adherence to prescribed medications are essential for long-term survival. Maintaining a healthy lifestyle after the operation helps protect the transplanted organ. Many specialized medical centers report high survival rates, especially within the first five years. Today, Liver transplant is widely recognized as an effective treatment for end-stage liver disease. Regular medical checkups play a key role in ensuring lasting success and a better quality of life.
Types of liver transplant
An orthotopic transplant
An orthotopic liver transplant is a type of surgery in which the patient’s diseased liver is removed and replaced with a healthy liver from a donor. The term “orthotopic” refers to the fact that the new liver is placed in the same location in the body as the patient’s original liver.
Living donor transplant
A living donor liver transplant is a type of surgery in which a portion of the liver is removed from a healthy living donor and transplanted into a recipient who has end-stage liver disease or liver failure.
Split type liver transplant
A split liver transplant is a type of surgery in which a single donated liver is split into two parts and transplanted into two different recipients. This procedure can potentially increase the number of available donor organs and improve access to transplantation for patients on the waiting list.
Auxiliary liver transplantation
Auxiliary liver transplantation involves transplanting a portion of a healthy liver from a living or deceased donor into the recipient’s body to support their diseased liver. Medical professionals perform this surgery in cases where the recipient’s liver is not completely dysfunctional but is insufficient to meet the body’s metabolic needs.
before and after liver transplant
Who is eligible for a liver transplant surgery?
Liver transplantation is a complex procedure, and determining if someone is a suitable candidate for the procedure requires a thorough evaluation by a transplant team. In general, medical professionals consider liver transplantation for individuals with end-stage liver disease or liver failure that cannot be effectively managed with other treatments, such as medication or surgery.
Some of the conditions that may lead to liver transplantation include:
- Acute liver failure
- Chronic liver diseases, such as cirrhosis, hepatitis B or C, primary biliary cirrhosis, or primary sclerosing cholangitis
- Metabolic liver diseases, such as Wilson’s disease, hemochromatosis, or alpha-1 antitrypsin deficiency
- Liver cancer
UPMC Living-Donor Liver Transplant
Liver Transplant
What are the criteria for a liver transplant?
- Clinical Signs of Liver Failure or Primary Liver Cancer: Individuals who have advanced liver disease, cirrhosis, or primary liver cancer are often considered for liver transplantation. The severity of the liver condition is assessed through various medical tests and evaluations.
- Surgical Suitability and Recovery: Candidates must be in a condition where they can undergo major surgery and have a reasonable chance of recovering well post-transplantation. This involves assessing the overall health and fitness of the individual.
- Absence of Future Substance Abuse Risk: Transplant teams are cautious about selecting candidates who may pose a risk of future alcohol or drug abuse. This is because continued substance abuse can jeopardize the success of the transplant and the overall health of the recipient.
What is the success rate of liver transplantation?
The success rate of liver transplantation is generally high, with a significant percentage of patients experiencing improved quality of life and long-term survival. The success of a surgery can be influenced by various factors, including the overall health of the recipient, the cause of liver disease, the type of transplant (living or deceased donor), and the expertise of the medical team.
In general, survival rates one year after liver transplantation are typically around 85% to 95%, and the five-year survival rates can range from 70% to 80% or higher, depending on the specific circumstances. Advances in surgical techniques, immunosuppressive medications, and post-transplant care have contributed to improved outcomes over the years.
What are the evaluations before liver transplantation?
Before undergoing liver transplantation, patients undergo thorough evaluations to ensure the procedure’s suitability and increase the chances of success. The evaluations include:
Medical Evaluation: This involves a detailed assessment of the patient’s medical history, current medications, and a series of diagnostic tests such as blood tests and imaging studies. The focus is on evaluating the overall health of the liver and other organs.
Psychosocial Evaluation: A psychosocial evaluation assesses the patient’s emotional and psychological wellbeing. It identifies any social or financial factors that may impact the success of the transplant.
Transplant Committee Review: The patient’s case is reviewed by a transplant committee comprising medical professionals from different specialties. This review determines if the patient is a suitable candidate for liver transplantation.
Liver transplant operation: step by step
how long does a liver transplant last?
The prognosis for individuals undergoing liver transplantation is typically positive. Over 90% of recipients survive beyond the first year, and approximately 80% continue to live for at least 5 years. Moreover, a substantial number of people enjoy a life that extends well beyond two decades or more after the transplant.
This indicates the success and longevity of surgery outcomes, highlighting the effectiveness of medical advancements in transplantation procedures, postoperative care, and immunosuppressive therapies.
Is there an age limit for liver transplantation?
There is no absolute age restriction for liver transplantation, as medical professionals evaluate each case individually based on the patient’s overall health and other medical conditions. However, age can significantly influence the determination of candidacy for the procedure, as older patients may face a higher risk of complications associated with the transplantation process.
Is liver transplant possible for children?
Yes, children can undergo liver transplantation and may be candidates for the procedure in cases where they have end-stage liver disease or liver failure that cannot be managed with other treatments.
Is donor and recipient blood type compatibility necessary in transplantation?
Yes, it is essential for the blood type of the donor and the patient to be compatible for a surgery to be successful. Blood type incompatibility can lead to a serious immune reaction that can cause the body to reject the transplanted liver.
How is the operation of liver transplantation?
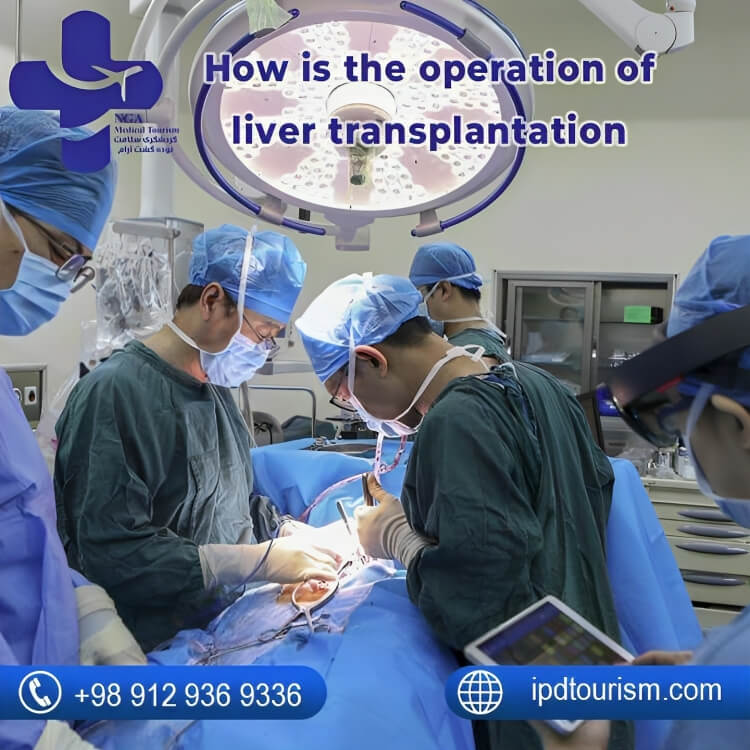
This surgery, like most organ transplant surgeries, is a complex procedure that usually takes several hours and requires a team of experienced surgeons and medical specialists.The procedure involves the following general steps:
Anesthesia: Medical professionals administer general anesthesia to ensure the patient is completely asleep and pain-free during the procedure.
Incision: The surgeon makes an incision in the upper abdomen to access the liver. The size and location of the incision may vary depending on the patient’s individual circumstances.
Liver removal: The surgeon carefully removes the patient’s diseased liver, preserving the blood vessels and bile ducts that will later be used to connect the new liver.
Donor liver preparation: If the liver is from a deceased donor, medical professionals carefully prepare the donor liver for transplantation. This process includes removing any unnecessary tissue and preserving the blood vessels and bile ducts.
My experience with liver transplantation in Iran
What is diet after liver transplantation?
After surgery, the body requires additional protein to support the healing process. Excellent sources of protein include lean meats, poultry, fish, eggs, dairy products, beans, and nuts.
Following surgery, doctors typically recommend a low-fat diet for patients to prevent complications such as high blood pressure, high cholesterol, and weight gain. Beneficial sources of low-fat foods encompass fruits, vegetables, whole grains, lean proteins, and low-fat dairy products.
Patients should abstain from alcohol post liver transplant surgery to prevent damage to the newly transplanted liver and interference with prescribed medications.
To manage potential digestive issues and maintain a healthy weight, patients may receive advice on consuming smaller, more frequent meals.
To promote overall health and prevent dehydration, healthcare providers typically encourage patients to consume abundant water and other beverages that are non-alcoholic and non-caffeinated.
Points to follow after liver transplant
After a liver transplant, patients are advised to follow several crucial points to ensure a successful recovery and maintain the health of the transplanted organ. Here are some key guidelines:
- Avoid Smoking:
- Stay Hydrated
- Monitor for Signs of Rejection
- Psychological Support
- Compliance with Lifestyle Recommendations
- Medication Adherence
- Regular Medical Follow-ups
- Healthy Lifestyle
- Hygiene and Infection Prevention
- Limit Alcohol Consumption
What is liver transplant bypass?
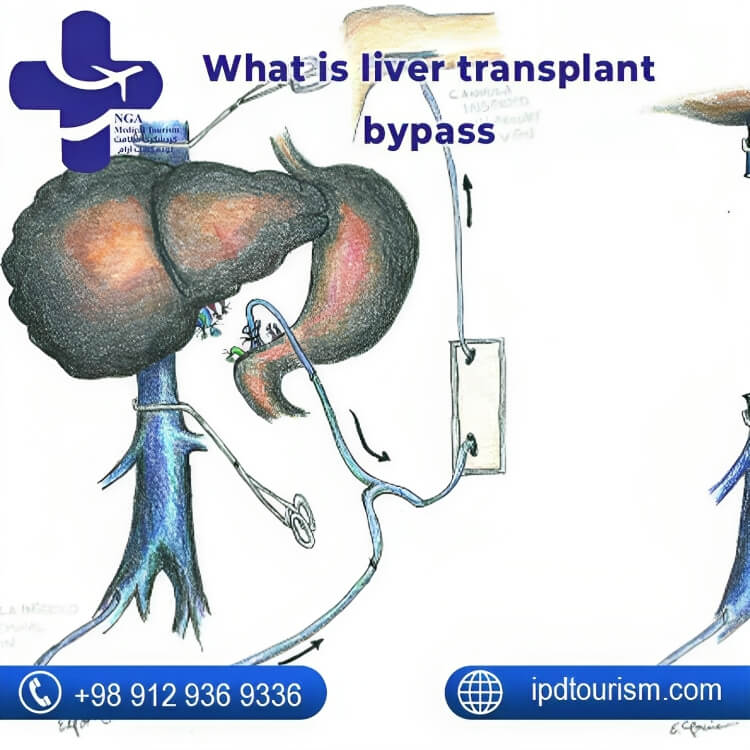
The use of a veno-venous bypass in liver transplantation is a controversial yet sometimes necessary procedure. Clamping major veins during general surgery can decrease blood returning to the heart, potentially impacting blood pressure and vital organ perfusion.
The veno-venous bypass redirects blood through an external circuit, bypassing clamps, and ensuring a safer surgical environment. While associated with complications, this technique is often considered the safest option to maintain adequate blood flow during liver transplantation.
What are the complications of liver transplant surgery?
Rejection
The patient’s immune system may recognize the new liver as a foreign object and try to attack it. This can lead to rejection of the new liver, which can cause damage and potentially lead to failure of the transplant.
Infection
Patients are at an increased risk of infection after transplant surgery due to the use of immunosuppressive medications to prevent rejection. Infections can occur in the incision site, urinary tract, lungs, or other areas of the body.
Bile duct complications
The anastomoses used to connect the bile ducts of the new liver to the patient’s existing biliary system can sometimes result in complications, such as bile leaks or strictures.
Cardiovascular complications
Patients may experience cardiovascular complications after surgery, such as high blood pressure, heart attack, or stroke.
Bleeding
The surgical incision made during surgery surgery can bleed, and patients may require blood transfusions in rare cases.
Kidney dysfunction
Patients may experience kidney dysfunction after surgery, which can cause fluid buildup, electrolyte imbalances, and other complications.
Metabolic complications
Patients may experience metabolic complications after surgery, such as diabetes, high cholesterol, or obesity.
What Is Liver Transplant Rejection?
transplant failure or rejection occurs when the patient’s immune system recognizes the donor liver as a foreign object and tries to attack it. This can cause damage to the new liver, impair its function, and potentially lead to failure of the transplant.
Warning signs after a liver transplant
liver rejection is a serious complication that can occur after surgery. The signs and symptoms of liver rejection may vary depending on the severity of the rejection, but some common signs to look out for include:
- Fever and chills
- Fatigue and weakness
- Pain or tenderness in the area of the surgery
- Nausea and vomiting
- Loss of appetite
- Jaundice (yellowing of the skin and eyes)
- Dark urine or light-colored stools
- Abdominal swelling or fluid accumulation
- Elevated liver enzyme levels
Ways to prevent liver transplant rejection
To prevent liver rejection after surgery, patients are typically prescribed immunosuppressive medications. These medications work by suppressing the immune system and preventing it from attacking the new liver.
The specific medications and dosages may vary depending on the patient’s individual circumstances and medical history, and the transplant team will carefully monitor the patient’s response to the medications and adjust the regimen as needed.
Who is not eligible for a liver transplant?
Several medical conditions may serve as surgery exclusion criteria, meaning they can disqualify a person from being considered for surgery. Some of these conditions include:
- Active substance abuse: Patients actively using drugs or alcohol.
- Untreated infections: Patients with untreated infections may face exclusion from surgery.
- Advanced cancer: Patients with cancer that has advanced beyond the liver may be excluded from surgery.
- Severe heart or lung disease: Patients with severe heart or lung disease may face exclusion from surgery due to the increased risk of complications and the potential for poor outcomes.
- Active sepsis: Patients with active sepsis, a potentially life-threatening condition caused by infection, may be excluded.
- Severe neurological impairment: Patients with severe neurological impairment may be excluded from surgery.
pediatric liver transplant
Pediatric liver transplant is a specialized procedure designed for children with severe liver disease or congenital liver defects. Careful evaluation is essential to ensure the child is a suitable candidate for surgery. The operation involves replacing the diseased liver with a healthy donor organ, which can come from a living or deceased donor. Postoperative care is critical, including the use of medications to prevent organ rejection and close monitoring of growth and development. Families play a key role in supporting recovery and maintaining follow-up appointments. Early intervention can significantly improve quality of life and long-term outcomes. Liver transplant offers children with life-threatening liver conditions a chance for a healthy, active future.
Can a person with cirrhosis of the liver get a liver transplant?
Yes, individuals with cirrhosis of the liver can be eligible for a surgery. transplantation is a common treatment for end-stage liver disease, including cirrhosis, offering a chance for improved health and extended life. Eligibility depends on factors such as overall health, severity of cirrhosis, and adherence to medical recommendations.
How long can a liver wait to be transplanted?
The waiting period for a surgery from a deceased donor can vary widely, ranging from less than 30 days to over 5 years. The duration depends on factors such as the availability of donor organs, the patient’s medical condition, and the organ allocation system in place.
Liver transplant waiting list
The waiting list for a liver transplant is often long due to the limited availability of donor organs. Patients are prioritized based on the severity of their liver disease and overall health condition. While waiting, regular medical check-ups are essential to track any changes in their condition. Maintaining a healthy lifestyle and following medical guidance can improve the chances of a successful surgery. Emotional and psychological support plays a key role in coping with the stress of waiting. When a suitable donor becomes available, timely notification and preparation are critical. Close communication with the transplant center ensures the best possible outcome for each patient.
liver cancer and liver transplant
Liver cancer is a serious condition that can severely damage liver function and limit treatment options. In selected cases, surgical intervention may be necessary to remove the tumor or replace the diseased liver. Careful evaluation is required to determine if a patient is eligible for a liver transplant, considering factors such as tumor size and overall health. Early detection and ongoing medical monitoring improve the chances of successful treatment. Patients often need additional therapies, such as chemotherapy or targeted treatments, before or after surgery. Maintaining a healthy lifestyle and following medical advice are crucial for recovery and long-term survival. Liver transplant can offer a life-saving solution for those with advanced liver cancer when other treatments are not sufficient.
cost of liver transplant in Iran : how much is liver
Iran has emerged as a sought-after destination for transplants, offering top-notch results at remarkably affordable prices. The entire procedure, from evaluation to surgery and postoperative care, can be obtained for approximately $100,000. This competitive cost, coupled with high standards of medical expertise, has attracted individuals seeking liver transplantation.
Iran’s healthcare system, equipped with advanced facilities and skilled medical professionals, provides an accessible option for those in need of this life-saving procedure without compromising on quality.
Conclusion:
Liver transplants offer a vital lifeline to those with end-stage liver diseases, granting renewed health and improved quality of life. Despite success, the organ shortage underscores the urgency for research, better organ preservation, and heightened public awareness about donation to enhance outcomes and save lives. While kidney transplants address a different set of health issues, the overall need for organ donors remains a pressing concern across various transplant fields.
Read More: Lasik eye surgery in Iran Question and Answer
Read More: Eye Surgery cost in Iran (Lasik&Refractive Surgery,Cataract)
Read More: lasik Eye Surgery in Iran
Read More: Glaucoma Treatment In Iran
Read More: Cataract surgery in Iran
FAQ:
The surgeon removes the gallbladder along with the diseased liver, as the donor liver comes with gallbladder attached, because it stores bile for the liver. Therefore, the transplant surgeon removes it before transplanting the liver.
Doctors recommend a liver transplant for people with early liver cancer, especially those who also have severe cirrhosis, or scarring of the organ. However, a transplant is usually reserved for people with liver cancer who have 1 tumor that is up to 5 centimeters in diameter, or 2 or 3 tumors that are each less than 3 centimeters in diameter. A transplant is not an option when the cancer has metastasized or spread to other parts of the body.
Liver transplant is the only effective treatment for Hepatitis B patients, as in most cases, hepatitis B causes liver cancer or severe damage to the liver, resulting in end-stage liver disease and ultimately liver failure.
The short-term survival rate (5-year) for patients who have had a transplant is between 60% and 70%. However, patients infected with either hepatitis B or hepatitis C will be treated with antiviral medicines before the transplant and after the surgery for a certain amount of time to prevent the healthy liver from becoming infected.
An interchangeable medical ID is composed of a bracelet strand with a lobster clasp at either end and a removable medical ID tag. Medical ID bracelets provide a quick way to communicate important health information to first responders in case of an emergency.
Heavy immunosuppression with tacrolimus, mycophenolate mofetil, and/or sirolimus may reverse chronic rejection in early phases.
Although there no studies to support that, vitamin K is frequently administered in an attempt to correct the elevated PT/INR levels that are often seen in cirrhotic patients.
In general, drinking alcohol after liver transplant is not recommended even for people who have not had alcohol-related liver disease.
A liver transplant recipient should not take acetaminophen (Tylenol) or aspirin for a fever, unless it is approved by transplant coordinator.
The short answer is no transplanted organs do not last forever. However, a transplanted liver will function for five years or more in 70 percent of recipients, and even longer if the organ came from a living donor.
Liver transplantation does not always cure hepatitis B as the virus is still in the blood after the transplant.
Liver transplantation effectively cures this disease, with a long-term survival rate of about 80%.